The Ultimate 15-Step Guide to Effective Health History Assessment in Nursing | studycreek.com
Learn the final 15 step Health History Assessment in nursing Guide.
Studycreek.com can teach you how nurses can gather valid subjective data, enhance patient outcomes, and enhance clinical decision-making with the help of expert advice.
Introduction
In contemporary healthcare, proper assessment of a patient is done way before using physical examination tools. Health History Assessment in Nursing is the basis of safe, effective, and patient-centered care. The critical nursing procedure enables clinicians to develop valuable subjective information, interpret patient experiences, and determine health priorities that affect the planning of care.
It is of paramount importance to master Health History Assessment in Nursing among nursing students and practicing professionals. It reinforces clinical judgment, improves communication and helps provide holistic care to patients.
StudyCreek.com provides nursing learners with advanced academic assistance to master difficult nursing concepts of health evaluation, clinical records, and reflection-on-practice.
This study will cover the significance, elements, and excellence of Health History Assessment in Nursing that will enable you to gain confidence and proficiency in this essential skill.
Defining: What Is Health History Assessment in Nursing?
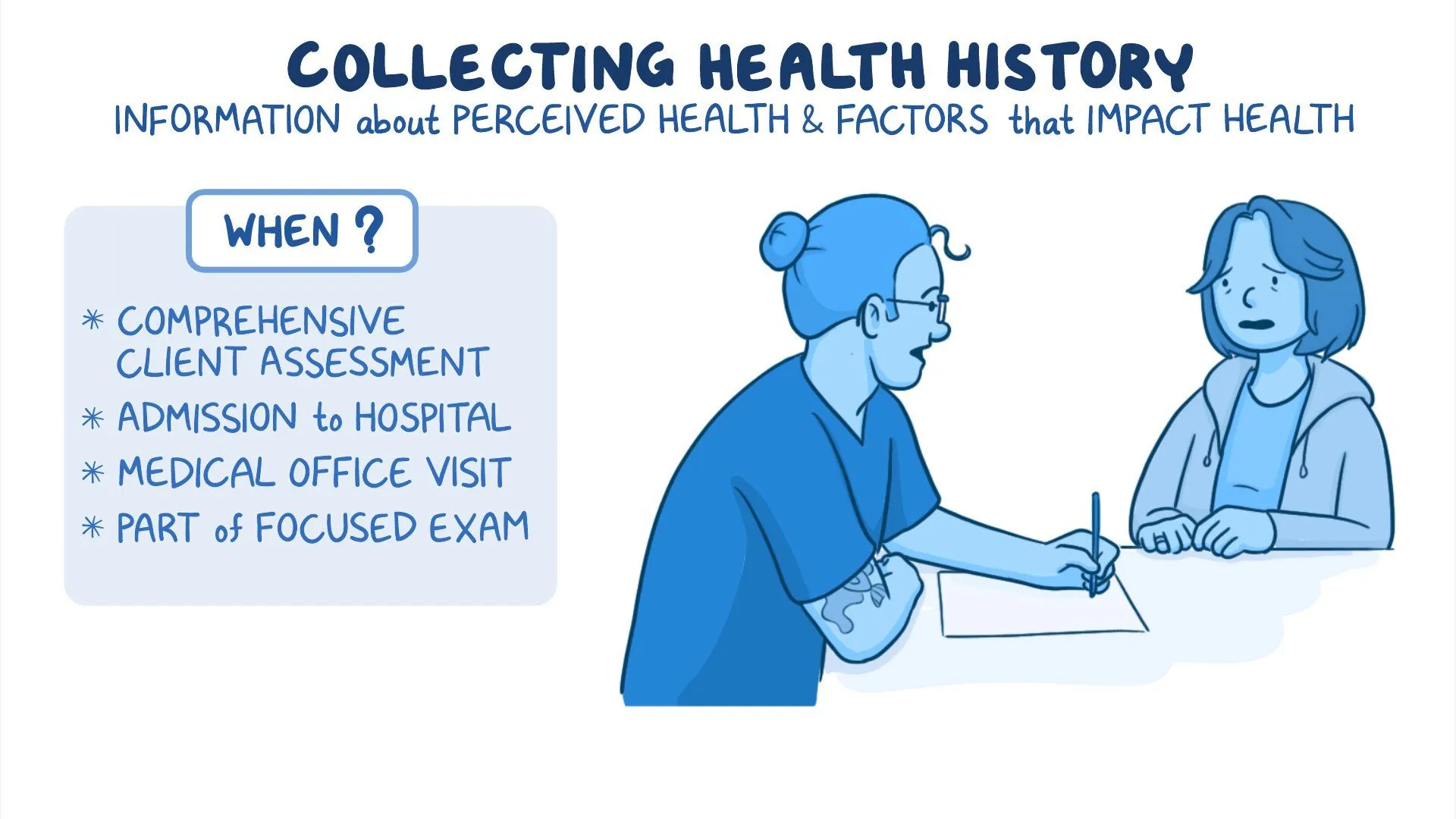
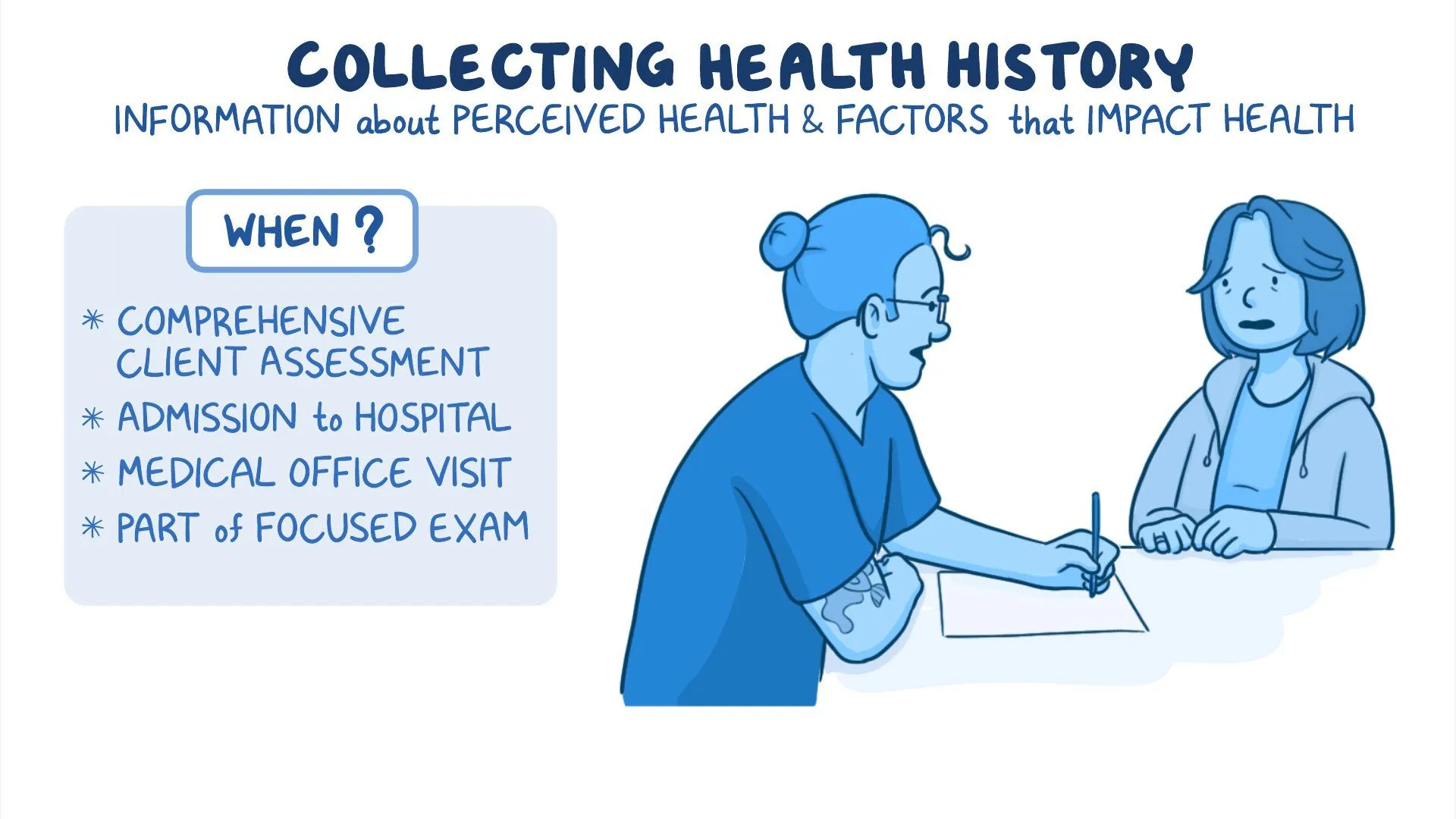
The Nursing process of gathering subjective information directly through the patient and is a systematic process called Health History Assessment. It deals with individual perceptions, experience, beliefs and concerns of health and illness.
Subjective data is based on patient self reporting unlike objective data which is observed or measured. This brings communication competence, empathy and belief as the core of effective Health History Assessment in Nursing. The data obtained is the foundation of the development of nursing diagnoses, intervention plans, and wellness.
The importance of Health History Assessment in Nursing Why Health History Assessment is important in Nursing.
Health History Assessment is an essential part of Nursing. It enables nurses to:
- Determine real and possible health issues.
- Identify risk factors at an early stage.
- Learn about psychosocial and cultural factors.
- Encourage patient-centred care.
- Increase safety and continuity of care.
By using the extensive Health History Assessment in Nursing, nurses are able to understand the entire person, not only the symptoms, and thus, they obtain better results and improve the relationships between nurses and patients.
The 15 Essentials of Health History Assessment in Nursing.
1. Demographic Data
The assessment is contextualized by the basic information on age, gender, occupation, and living situation.
2. Perception of Health
The Health History Assessment in Nursing involves understanding of how the patients perceive themselves in terms of health.
3. Chief Concern
This defines the main motive of seeking care as was mentioned by the patient.
4. History of Present Illness
An overview of when the symptoms occurred, how long and how it has affected his daily life.
5. Past Medical History
Past diseases, hospital stay, operations and vaccinations guide risk evaluation.
6. Medication History
There should be a review of prescription, non-prescription and herbal drugs.
7. Allergy History
Necessary in order to avoid negative reactions and guarantee patient safety.
8. Family Medical History
The genetic and hereditary patterns are very important in Health History Assessment in Nursing.
9. Review of Systems
Head-to-toe examination can be done to make sure that no symptoms are missed.
10. Nutritional History
Food culture determines the risk of chronic diseases and well-being.
11. Sleep and Rest Patterns
The quality of sleep has direct influence on both the physical and mental well-being.
12. Activity and Exercise
Health promotion strategies are based on mobility and fitness levels.
13. Psychosocial Assessment
The main aspects of Health History Assessment in Nursing are mental health, stressors, and coping mechanisms.
14. Cultural and Spiritual Considerations.
Healthcare decisions and acceptance of the treatments depend on beliefs.
15. Developmental Considerations
The application of age-related functioning evaluation with the help of frameworks, such as the Erikson stages, can benefit nurses.Nursing Health History Assessment Communication Skills.
Nursing requires effective Health History Assessment which relies on therapeutic communication. Open-ended questions, active listening, and nonjudgmental responses should be applied by nurses to facilitate honesty and trust.
Data accuracy can be influenced by barriers like language difference, anxiety or even cultural misunderstanding. The ability of nurses to adjust their communication strategy to address these issues and make the assessment accurate is a skill that skilled nurses develop.
Whole Person Care and Health History assessment in Nursing.
Holistic nursing acknowledges the fact that health is determined by the physical, emotional, social and spiritual factors. In Nursing, Health History Assessment can be helpful in providing holistic care since it helps in the combination of all the aspects of life of the patient in clinical decision-making.
This methodology will lead to better patient interaction, appreciation of personal values, and long-lasting health instead of symptom-oriented care only.
Documentation and Professional Responsibility.
Professional and legal documentation is an aspect of Health History Assessment in Nursing. Clear, concise, and factual documentation facilitate continuity of care and safeguard both the patients and health care providers.
Nurses should uphold confidentiality, ethical behaviour and adherence to professional standards when recording health histories.
Routine Problems in Nursing in Assessing Health History.
Health History Assessment in Nursing is a challenging task despite its significance and has the following challenges:
- Time constraints
- Failure to respond fully on the part of the patient.
- Emotional discomfort
- Cultural barriers
These issues can be conquered through practice, thinking, and the continuous development of the professional.
Value in Education to Nursing Students.
Health History Assessment in Nursing is the interface between theory and practice to the students. It builds critical thinking, clinical reasoning and confidence when dealing with patients. StudyCreek.com is an academic resource that assists nursing students in their research by providing them with professionally developed papers, case studies, and evaluations based on the academic requirements.
Application of Technology to improve Health History Assessment in Nursing.
Health History Assessment in Nursing has been changed due to the use of electronic health records and digital assessment tools. There is no denying that technology has enhanced efficiency, however, the nurses should not overlook the importance of interacting with the patient to ensure proper collection of subjective data.
Health History Assessment in Nursing: Career Impact of Mastering It.
Nurses who master Health History Assessment in Nursing are better in clinical judgment, leadership potential and patient advocacy skills. Such are competencies that have been so desirable in the healthcare environments.
Professional Support and Resources-External.
Academic and technical help is popular among nursing professionals and students to improve the skills of assessment. These platforms such as
Workvix.com also offer external professional services that help in functioning learning, research, and project development in healthcare and related sectors.
Conclusion
Nursing Health History Assessment is one of the pillars of safe, effective, and caring care. It will enable nurses to conceptualize patients comprehensively, determine their health priorities, and provide more personalized interventions. The skill will improve patient outcomes, professional confidence and clinical excellence.
Assessment skills are important to invest in, either as a nursing student or a professional. By having the academic assistance of StudyCreek.com, it will be possible to master the Health History Assessment in Nursing in an efficient, effective, and rewarding manner.

SAMPLE QUESTION
Purpose
Before any nursing plan of care or intervention can be implemented or evaluated, the nurse assesses the individual through the collection of both subjective and objective data. The data collected are used to determine areas of need or problems to be addressed by the nursing care plan. This assignment will focus on collecting subjective assessment data, synthesizing the data, and on identifying health/wellness priorities based on the findings. The purpose of the assignment is two-fold:
· To recognize the interrelationships of subjective data (physiological, psychosocial, cultural/spiritual, and developmental) affecting health and wellness.
· To reflect on the interactive process between self and client when conducting a health assessment.
Course Outcomes: This assignment enables the student to meet the following course outcomes:
CO 1: Explain expected patient behaviors while differentiating between normal findings, variations, and abnormalities. (PO 1)
CO 2: Utilize prior knowledge of theories and principles of nursing and related disciplines to integrate clinical judgment in professional decision-making and implementation of the nursing process while obtaining a physical assessment. (POs 4 and 8)
CO 3: Recognize the influence that developmental stages have on physical, psychosocial, cultural, and spiritual functioning. (PO 1)
CO 4: Utilize effective communication when performing a health assessment. (PO 3)
CO 5: Demonstrate beginning skill in performing a complete physical examination, using the techniques of inspection, palpation, percussion, and auscultation. (PO 2)
CO 6: Identify teaching/learning needs from the health history of an individual. (POs 2 and 5)
CO 7: Explore the professional responsibilities involved in conducting a comprehensive health assessment and providing appropriate documentation. (POs 6 and 7)
Due date: Your faculty member will inform you when this assignment is due. The Late Assignment Policy applies to this assignment.
Total points possible: 100 points
Preparing the assignment
Follow these guidelines when completing this assignment. Speak with your faculty member if you have questions.
1. Complete a health assessment/history on an individual of your choice who is 18 years of age or older and NOT a family member or close friend.
a. The purpose of this restriction is to avoid any tendency to anticipate answers or to influence how the questions are answered. Your goal in choosing an interviewee is to simulate the interaction between you and an individual for whom you would provide care.
b. Inform the individual that information obtained will be kept confidential and do not use identifying information within the assignment.
2. Include the following sections when completing the assignment.
a. Health History Assessment (70 points/70%)
1) Demographics
2) Perception of Health
3) Past Medical History
4) Family Medical History
5) Review of Systems
6) Developmental Considerations- use Erikson’s Stages of Psychosocial Development- which stage is your participant at and give examples of if they have met or not met the milestones for that stage.
7) Cultural Considerations- definition, cultural traditions, cultural viewpoints on healing/healers, traditional and complementary medicine, these are examples but please add more
8) Psychosocial Considerations- support systems-family, religious, occupational, community these are examples but please add more
9) Collaborative Resources to Improve Health- give examples of resources available to improve the health of the participant such as community, nutritional recommendations, healthcare, spiritual, etc.
b. Reflection (20 points/20%)
Reflection is used to intentionally examine our thought processes, actions, and behaviors in order to evaluate outcomes. Provide a written reflection that describes your experience with conducting this Health History.
1) Reflect on your interaction with the interviewee holistically.
a) Describes the interaction in its entirety: include the environment, your approach to the individual, time of day, and other features relevant to therapeutic communication and to the interview process.
2) How did your interaction compare to what you have learned?
3) What barriers to communication did you experience?
a) How did you overcome them?
b) What will you do to overcome them in the future?
4) What went well with this assignment?
5) Were there unanticipated challenges during this assignment?
6) Was there information you wished you had available but did not?
7) How will you alter your approach next time?
3. Style and Organization (10 Points/10%)
Your writing should reflect your synthesis of ideas based on prior knowledge, newly acquired information, and appropriate writing skills. Scoring of your work in written communication is based on proper use of grammar, spelling, APA, and how clearly you express your thoughts and reasoning in your writing.
1) Grammar and mechanics are free of errors.
2) Verbalizes thoughts and reasoning clearly.
3) Uses appropriate resources and ideas to support topic with APA where applicabl
ANSWER
Health History Evaluation and Reflection.
Health History Assessment
Demographics
The patient is a 29-year-old adult female. She is an African who lives in an urban area. She is unmarried, she works full-time as an administrative assistant, and has post-secondary education. The respondent has enough time and money to live in a rented apartment on her own and has access to the basic needs such as utilities, transport, and healthcare services. No identifying information is presented to ensure confidentiality.
Perception of Health
The respondent states that she is generally healthy but stressful. She denies physical health issues and claims that she feels good most of the days, but she experiences frequent fatigue due to work-related stress and irregular sleep habits. Her health, she thinks, would be better in terms of stress management, physical activity, and diet. She states that she is serious when it comes to seeking medical attention when necessary but notes that she puts off regular checkups because of lack of time.
Past Medical History
The subject denies any chronic diseases like high blood pressure, diabetes, asthma, or heart disease. She denies having never been vaccinated or having any health issues with her childhood vaccinations, and denies not having regular vaccinations, although she is an adult. She denies that she had any surgeries or hospitalizations. The patient denies stress-related headaches and does not take prescription drugs. She sometimes takes analgesics that are available on the counter to relieve headaches. No reported drug or food allergies.
Family Medical History
The participant indicates that her mother is alive but has hypertension which is treated with medication. Her father is also alive and he has type 2 diabetes. She denies a sibling that is healthy and has no known medical history. No family history of cancer, stroke, mental illness and genetic disorders. The history of cardiovascular and metabolic diseases in later life puts the participant at risk because of this family history.
Review of Systems
The subjective findings the participant mentions are as follows:
General: Fatigue, particularly after working long hours; no loss of weight or fever of unknown etiology.
Skin: no rashes, lesions, itching; denies skin defects.
Head and Neck: That periodically experiences tension headaches, no dizziness or neck stiffness.
Eyes: No visual defects, wears corrective glasses with mild myopia.
Ears: No deafness, ringing in ears, ear pain.
Nose and Throat: No stuffiness, sore throat, or dysphagia.
Lung: Denies breathlessness, cough or wheezing.
Cardiovascular: Denies any chest pain, palpitations or edema.
Gastrointestinal: Infrequent bloating with an irregular intake of food; regular bowel movements.
Genitourinary: No dysuria, frequency, or urgency; reports regular menstrual periods.
Musculoskeletal: The back of the lower back pain infrequently, following excessive sitting at work.
Neurological: Denies numbness, tingling or weakness.
Psychological: Denies depression or sleeping problems, reports work-related stress and occasional anxiety.
Developmental Considerations (Psychosocial Development of Erikson)
As per Erikson stages of psychosocial development, the participant is at Intimacy vs. Isolation stage, which normally happens in the stage of young adulthood. This phase is concerned with the establishment of intimate relationships and emotional attachment towards other people.
The participant exhibits effective accomplishment of this phase by having close friendship ties, engaging in social life and intending on the need to have romantic relationships that have meaning. She however also reports of being emotionally withdrawn in the instances of stress, which indicates some partial difficulties in balancing intimacy and independence. All in all, the participant seems to be developing well in this developmental stage.
Cultural Considerations
Culture can be defined as that of the beliefs, values, practices and customs that are shared and that affect the health practices and perceptions of an individual. The participant is closely connected with her culture and tells that family cohesion and respect towards older people are valued values.
She states that home remedies are sometimes applied to minor illnesses with the use of traditional home remedies like herbal teas. Although she admires the traditional form of healing, she mostly uses the modern medical services when seeking medical care. The participant thinks that healing is a blend of physical nurturing, emotional and spiritual health. She says she is open to alternative medicine but stresses the need for evidence based care.
Psychosocial Considerations
The respondent also indicates that she has an excellent support system, comprising of her close friends, extended family members, and workmates. She recognizes her mother as her motherly source of support. She works full-time and she reports moderate job satisfaction and high levels of stress.
The participant is religious spiritually, and according to her, prayer and faith are sources of emotional relief on tough days. She engages in community works via her place of worship and this has a positive effect on her sense of belonging and inner peace.
Cooperation Resources to enhance Health.
There are a number of materials that can be used to assist the health and wellness of the participant. These entail availability of primary healthcare services in regard to preventive screenings and health education. Nutritional counseling may help her to make healthier eating habits. Regular work outs or low priced gym memberships may encourage physical exercise.
Mental health services, including stress management courses or counseling, can be used to deal with work-related stress. Religious support with her religious community is also a good source of emotional and psychological health.
Reflection
The experience of making such a health history assessment was a positive learning activity that helped me to better understand the interaction of the nurse and the client. The interview was conducted in a very private environment during the early evening time, this made the interviewer relaxed and comfortable. My tone was relaxed, body language was open and I used therapeutic communication methods thanks to which I was able to build trust and make them open up.
This interaction was closely related to what I have studied in classes regarding holistic assessment and patient-centered care. Throughout the interview, I was able to combine active listening, empathy, and open-ended questioning. It has been found that the lack of fluency in talking about stress and emotional well-being is one of the barriers to communication that occurs occasionally among the participant. I did this by assuring, keeping eye contact and giving time to reflect.
The positive thing as part of this assignment was that I was also able to be professional and connect with the rapport. I could collect in-depth subjective data without haste during the interview process. The other unexpected difficulty was time management and having to cover every area needed in an extensive way.
I would have liked to know more about long-term health objectives of the participant, and this would have given me a better understanding of the wellness planning. Next time, I will use more specific questions concerning the goal-setting and lifestyle modifications. On the whole, the experience made me more confident in my ability to carry out health histories, as well as confirmed the relevance of holistic and culturally sensitive nursing care.
References
Erikson, E. H. (1968). Identity: Youth and crisis. New York, NY: Norton.
Jarvis, C. (2020). Physical examination and health assessment (8th ed.). Elsevier.